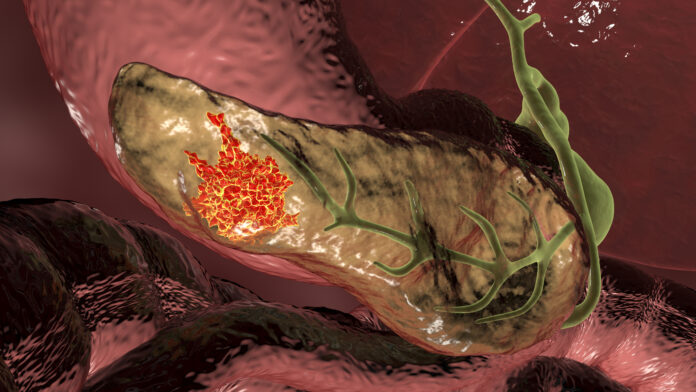
Investigators at Weill Cornell Medicine say they have identified a new potential pancreatic cancer treatment using an organoid model—lab grown tissues that mimic the geometry and function of the pancreas containing a common cancer driving mutation.
In their study, published Tuesday in the journal Cell Stem Cell, the researchers found that the cancer-driving mutation included in the organoid results in abnormally high production of cholesterol and that an old, little used the heart drug perhexiline maleate can significantly hindered this activity and, as a result, suppress the organoids’ growth.
“Our findings identify hyperactive cholesterol synthesis as a vulnerability that may be targetable in most pancreatic cancers,” said study co-senior author Todd Evans, MD, vice chair for research in surgery and a member of the Hartman Institute for Therapeutic Organ Regeneration at Weill Cornell Medicine.
Co-senior author Shuibing Chen, MD, director of the Center for Genomic Health, also a member of the Hartman Institute for Therapeutic Organ Regeneration at Weill Cornell Medicine added: This study also highlights the value of using genetically well-defined organoids to model cancer and discover new treatment strategies.”
While organoids that mimic the cell diversity and architecture of full-sized human and animal organs have been common tools for the study of disease and drug discovery, they can also be designed to mimic a diseased organ, such as the one Weill Cornell investigators used in the current study with a mutation that drives pancreatic cancer development. In this instance the researchers used normal mouse pancreatic tissue and engineered them to include the mutant gene KrasG12D, the mouse version of a cancer-driving mutant gene found in most cases of pancreatic ductal adenocarcinoma (PDAC).
Using these model organoids, the team tested more than 6,000 drugs, including drugs already approved by the U.S. Food and Drug Administration (FDA) and, based on the response of the organoids, identified several that showed they could markedly limit their growth. Among this small handful of drugs identified, the most promising was perhexiline maleate which is an approved drug to treat the heart condition angina in some regions of the world. Even a small dose of perhexiline maleate blocked growth of the organoids with mutated KrasG12D and in some cases killed them outright, while healthy organoids lacking the cancer-driving mutation exhibited no adverse effects when given the same dose.
This effect was caused, the researchers discovered, due to the Kras mutated gene driving increased production of cholesterol, which perhexiline maleate countered by inhibiting a key cholesterol metabolic pathway regulatory factor called SREBP2.
Cholesterol’s role in PDAC was not surprising to the investigators given an essential component needed for building cells and a promoter of cell survival, while it has also been shown to promote growth of certain tumor types, including lung cancer. Weill Cornell team’s findings now suggest that targeting cholesterol is a very promising new approach to combatting PDAC. Further, the ability of perhexiline maleate to thwart cancer growth in organoids possessing a range of Kras mutations suggests that targeting cholesterol could be broadly applicable as a treatment for KRAS-mutated cancers.
“We hope that our cholesterol-targeting strategy will be independent of particular KRAS mutations and will make it hard for treated tumors to evolve resistance,” Evans.
Despite its effectiveness in the model organoids, the researchers note that it is unlikely perhexiline maleate could be used as a treatment for PDAC, considering it can have serious side effects, including liver damage and peripheral nerve damage—which is why it was withdrawn from several European markets in the 1980s, and was never approved in the United States. The researchers will now use perhexiline maleate as the starting point to create a more refined PDAC treatment candidate and as tool for use in further studies of the role of cholesterol in PDAC development.













